Here, you can find all the information on the construction and validation of the Erlangen Test of Activities of Daily Living (E-ADL). If you have any further questions or suggestions, please do not hesitate to contact us.
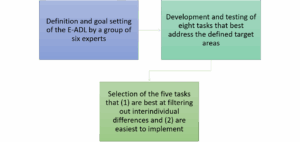
Item Construction
The E-ADL was developed and validated in three steps by Graessel et al. in 2009. The test was later revalidated by Luttenberger et al. (2012).
The first validation study of the E-ADL test was conducted in 2009 using a sample of 46 people with dementia living in nursing homes (42 women and four men). The average age was 85.9 years (SD = 6.6 years).
The Global Deterioration Scale (GDS; Reisberg et al., 1982; German version: Ihl & Fröhlich, 1991), the Mini Mental State Examination (MMSE; Folstein et al., 1975), and the Nurses Observation Scale for Geriatric Patients (NOSGER; Spiegel et al., 1991, 1992) were used to examine convergent validity.
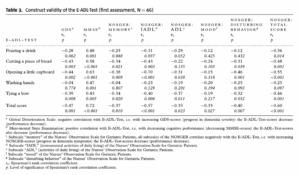
Moderate correlation coefficients between the total scores of the E-ADL test and the GDS, as well as the total scores of the MMSE and the NOSGER, confirmed the validity (see table below; Graessel et al., 2009):
Internal consistency: Cronbach’s alpha was .77.
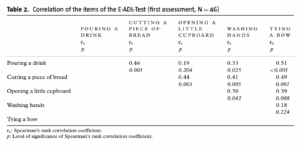
The correlations between the respective items are shown in the following table (see Graessel et al., 2009):
The test-retest reliability after 14 days of the entire test was .73 (p < .001). The following values were obtained for the individual items (see Graessel et al., 2009):
| Retest Reliability | |
| Pouring a drink | r = 0.35 (p = 0.024) |
| Cutting a piece of bread | r = 0.56 (p < 0.001) |
| Opening a small cupboard | r = 0.59 (p < 0.001) |
| Washing hands | r = 0.63 (p < 0.001) |
| Tying a bow | r = 0.48 (p = 0.001) |
Folstein, M. F., Folstein, S. E. andMcHugh, P. R. (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198.
Graessel, E., Viegas, R., Stemmer, R., Küchly, B., Kornhuber, J., & Donath, C. (2009). The Erlangen Test of Activities of Daily Living: first results on reliability and validity of a short performance test to measure fundamental activities of daily living in dementia patients. International Psychogeriatrics, 21(1), 103-112.
Ihl, R. and Fröhlich, L. (1991). Die Reisberg-Skalen GDS, CRS, FAST [The Reisberg Scales GDS, CRS, FAST], Weinheim: Beltz Test.
Reisberg, B., Ferris, S. H., Leon, M. J. de and Crook, T. (1982). The Global Deterioration Scale for assessment of primary degenerative dementia. American Journal of Psychiatry, 139, 1136–1139.
Spiegel, R. (1992). Erfassung des Verhaltens psychogeriatrischer Patienten im Alltag mit der NOSGER [Recording the behaviour of psycho-geriatric patients in daily life using NOSGER]. In N. I. Jovic and A. Uchtenhagen (eds.), Ambulante Psychogeriatrie: neue Wege und Hinweise für die Praxis [Outpatient Psychogeriatrics: New Ways and Tips]. Kröning: Roland Asanger Verlag.
Spiegel, R. et al. (1991). A new behavioral assessment scale for geriatric out- and inpatients: the NOSGER (Nurses’ Observation Scale for Geriatric Patients). Journal of the American Geriatrics Society, 39, 339–347.
A revalidation study of the E-ADL test followed in 2012 by Luttenberger et al. The sample consisted of 139 people with dementia from five nursing homes. They had an average age of 84.7 years (SD = 4.9 years), and 83% were women.
The Barthel Index, the ADAS-cog Scale, the Nurses Observation Scale for Geriatric Patients (NOSGER; Spiegel et al., 1991, 1992) and the Mini Mental State Examination (MMSE; Folstein et al., 1975) were used to examine validity.
Criterion-related validity was tested and confirmed using two hypotheses:
- H1: The E-ADL test result is positively correlated with the level of care at the beginning of the study. This correlation increases after 22 months. An eta of .39 (p < .001) at the beginning of the study and an eta of .48 (p < .001) after 22 months support H1.
- H2: An increase in the level of care during the observation period is associated with a greater decline in ADL abilities on the E-ADL test than in cases where the level of care does not change. An average 6-point decrease in ADL abilities on the E-ADL test with an increase in care level compared with a 2-point decrease in ADL abilities in the E-ADL test with no change in care level supports H2.
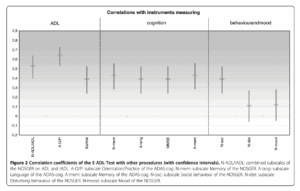
Construct validity was tested and supported with three hypotheses:
- H3: The strongest correlations between the E-ADL test and measurement instruments that measure ADLs (Activities of Daily Living) and IADLs (Instrumental Activities of Daily Living) are found in: (a) the NOSGER subscales “ADLs” and “IADLs,” (b) the ADAS-cog subscale “Orientation/Practice,” and (c) the Barthel Index.
- H4: Less pronounced correlations between the E-ADL test and measurement instruments that measure cognitive abilities can be observed in: (a) the NOSGER subscale “Memory,” (b) the ADAS-cog subscales “Speech” and “Memory,” and (c) the MMSE.
- H5: The weakest correlations between the E-ADL test and measurement instruments that measure behavior and mood are observed in: (a) the NOSGER subscale “Social behavior,” (b) the NOSGER subscale “Disturbing behavior,” and (c) the NOSGER subscale “Mood.”
Since eight of the 10 correlation coefficients supported H3 to H5, construct validity was considered to be established (see Luttenberger et al., 2012, Figure 2):
Internal consistency: Cronbach’s alpha for the entire sample was .68. In terms of the individual subgroups, Cronbach’s alpha was .37 for people with mild dementia, .64 for people with moderate dementia, and .73 for people with severe dementia.
Folstein, M. F., Folstein, S. E. andMcHugh, P. R. (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198.
Graessel, E., Viegas, R., Stemmer, R., Küchly, B., Kornhuber, J., & Donath, C. (2009). The Erlangen Test of Activities of Daily Living: first results on reliability and validity of a short performance test to measure fundamental activities of daily living in dementia patients. International Psychogeriatrics, 21(1), 103-112.
Ihl, R., & Fröhlich, L. (1991). Die Reisberg-Skalen GDS, CRS, FAST [The Reisberg Scales GDS, CRS, FAST].
Luttenberger, K., Schmiedeberg, A., & Gräßel, E. (2012). Activities of daily living in dementia: revalidation of the E-ADL test and suggestions for further development. BMC Psychiatry, 12, 1-10.
Reisberg, B., Ferris, S. H., Leon, M. J. de and Crook, T. (1982). The Global Deterioration Scale for assessment of primary degenerative dementia. American Journal of Psychiatry, 139, 1136–1139.
Spiegel, R. (1992). Erfassung des Verhaltens psychogeriatrischer Patienten im Alltag mit der NOSGER. Ambulante Psychogeriatrie, 28-42.
Spiegel, R. et al. (1991). A new behavioral assessment scale for geriatric out- and inpatients: the NOSGER (Nurses’ Observation Scale for Geriatric Patients). Journal of the American Geriatrics Society, 39, 339–347.
Given that interindividual variability and the validity parameters are difficult to differentiate in mild dementia, another performance test was developed for this target group to validly assess everyday practical skills: the Erlangen Test of Activities of Daily Living in Persons with Mild Dementia or Mild Cognitive Impairment (ETAM).
Erlangen Test of Activities of Daily Living (E-ADL); Activities of Daily Living (ADL)
