Here, you can find all the information on the construction and validation of the long version of the Burden Scale for Family Caregivers (BSFC) with 28 items. If you have any further questions or suggestions, please do not hesitate to contact us.
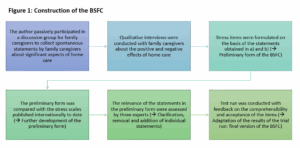
Item construction
The BSFC was developed and validated in six steps by Graessel in 2001. This was followed by an extended validation by Grau et al. in 2015.
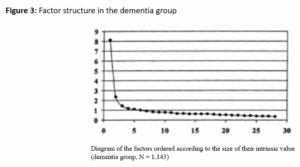
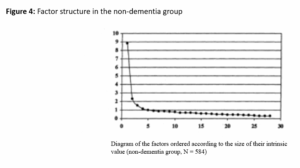
The validation of the BSFC was based on data from 1,911 informal caregivers (CGs). Of these, 1,253 CGs were caring for a dementia patient (M = 41.9, SD = 14.8). The nondementia group consisted of 612 people (M = 36.6, SD = 16.0). Subjective distress was significantly lower in the nondementia group (p < .001). Cronbach’s alpha was calculated to assess the internal consistency of the items, and a factor analysis was performed to determine the structure of the BSFC.
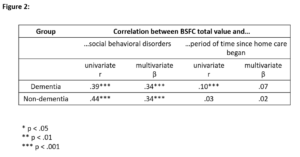
The BSFC sum value has demonstrated validity when measured against the criteria “social behavioral disorders” (convergent validity) and “time since home care began” (discriminant validity).
The internal consistency for the dementia sample was a Cronbach’s alpha of .90 (non-dementia group: Cronbach’s alpha = .91). When the survey was administered again after 14 days, the test-retest reliability was .94.
The interitem correlations in the dementia group were between -.21 and .55, with 63.5% of the values above .20. The interitem correlations in the non-dementia group were between -.13 and .57, with 76.5% of the values above .20.
Factor structure in the dementia group: 16 items with a value > .50 and six items with a value > .45 loaded on the general factor, explaining 29.1% of the variance.
Factor structure in the non-dementia group: 19 items with a value > .50 and three items with a value > .45 loaded on the general factor, explaining 31.5% of the variance.
Gräßel, E. (2001). Häusliche-Pflege-Skala HPS zur Erfassung der Belastung bei betreuenden oder pflegenden Personen. Ebersberg: Vless.
The extended validation of the BSFC was carried out using data from 351 CGs who were caring for a person with dementia at home (Grau et al., 2015). On average, the CGs were 59.2 years old (SD = 13.4), 73% were women, 31% were spouses or partners, 60% were children (in-law), and 9% were other kinds of CGs. The average age of those suffering from dementia was 80.3 years (SD = 6.7); 68% of them were women; 64% suffered from a mild form of dementia (Mini Mental State Examination (MMSE): 18-24 points; Folstein et al., 1975), and 36% from a moderate form (MMSE: 10-17 points). Cronbach’s alpha was calculated to determine the internal consistency of the items. A factor analysis was used to determine the correlation structure of the items. In addition, the discriminatory power, item difficulty, and construct validity were examined by testing five hypotheses.
In order to assess the validity of the scale, we analyzed additional information about the severity of dementia (MMSE; Folstein et al., 1975), demanding behaviors of dementia patients (Nurses’ Observation Scale for Geriatric Patients (NOSGER); Spiegel et al, 1991), the depression diagnosis of caregiving relatives (ICD-10 diagnosis, taken from health insurance data), the care level, the degree of care-recipient’s functional independence (Barthel Index; Mahoney, 1965), the care activities at night, the time required for informal care in hours per day (Resource Utilization in Dementia – Lite Version (RUD Lite); Wimo & Winblad, 2003), and socio-demographic and general characteristics.
Construct validity was tested and confirmed on the basis of five hypotheses (H1-H5). The results are presented in Table 3 in Grau et al. (2015).
- H1: The burden on CGs is positively correlated with the severity of cognitive impairment, which was measured with the MMSE.
- H2: Demanding behaviors (operationalized with the NOSGER “disruptive behavior” subscale) are among the most distressing symptoms associated with dementia. The burden on CGs is positively correlated with the severity of the challenging behaviors.
- H3: The burden on CGs is related to their mental health, that is, CGs with a diagnosis of a depressive episode have higher subjective burden scores than CGs without this diagnosis.
- H4: CGs who have only limited opportunities for retreat report a higher burden of care, that is, CGs who share an apartment/house with the person in need of care have a higher burden of care than those who live separately.
- H5: The more demanding the care requirement, the greater the burden on the CG.
- H5a: The higher the care level, the greater the burden on the CG.
- H5b: The lower the degree of independence of the care-recipient (measured with the Barthel Index), the greater the burden on the CG.
- H5c: The more care tasks are carried out at night, the greater the burden on the CG.
- H5d: The higher the average daily care effort in hours, the higher the CG´s workload.
Predictive validity was confirmed on the basis of H6: The higher the burden on the CG(s), the more likely it was that the care-recipient would be institutionalized in the future (transferred to a nursing home). All predictors are presented in Table 4 in Grau et al. (2015).
Internal consistency: Cronbach’s alpha was .92.
The item difficulty of the BSFC items ranged from .06 to .51. The discriminatory power of the items was between .10 and .75 (see Table 2 in Grau et al., 2015). Item 19 (“Bothered by outsiders”) showed the lowest discriminatory power of .10. For 26 items, the Cronbach’s alpha value “when the item was removed” was below the Cronbach’s alpha for the complete scale of .932. Two items had a Cronbach’s alpha value above .932 (Item 11: “Care not adequately acknowledged” and Item 19: “Bothered by outsiders”).
The exploratory factor analysis clearly indicated a one-factor structure for the BSFC. Although four factors had eigenvalues greater than 1.0 (see also Table 1 in Grau et al., 2015), the scree test indicated only one significant factor. This dominant factor explained 37% of the total variance, while the other three factors explained only 8%, 5%, and 4%, respectively. Nineteen items loaded strongly (factor loading > 0.5) and three items loaded moderately (factor loading > .45) on the dominant factor.
Folstein, M.F., Folstein, S.E. & McHugh, P.R. (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189-198.
Grau, H., Graessel, E. & Berth, H. (2015). The subjective burden of informal caregivers of persons with dementia: Extended validation of the German language version of the Burden Scale for Family Caregivers (BSFC). Aging & Mental Health, 19(2), 159-168.
Mahoney, F.I. & Barthel, D.W. (1965). Functional evaluation: The Barthel Index. Maryland State Medical Journal, 14, 61-65.
Spiegel, R., Brunner, C., Ermini-Fünfschilling, D., Monsch, A., Notter, M., Puxty, J. & Tremmel, L. (1991). A new behavioral assessment scale for geriatric out-and-in-patients: The NOSGER (Nurses´Observation Scale for Geriatric Patients). Journal of the American Geriatrics Society, 39(4), 339-347.
Wimo, A. & Winblad, B. (2003). Resource utilization in dementia: RUD Lite. Brain Aging, 3(1), 48-59.
The BSFC has been validated in the following languages: Danish, English, Turkish.
You can find the corresponding validation studies here.
Burden Scale for Family Caregivers (BSFC); Burden Scale for Family Caregivers – short form (BSFC-s); Informal Caregiver (CG); Arithmetic mean (m); Standard deviation (SD)
