Here, you can find all the information about the construction and validation of the short form of the Burden Scale for Family Caregivers (BSFC-s) with 10 items. If you have any further questions or suggestions, please do not hesitate to contact us.
Item Construction
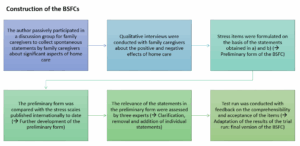
The BSFC-s was developed and validated in six steps by Graessel et al. in 2014. This was followed by an extended validation by Pendergrass et al. in 2018.
The first validation study of the BSFC-s took place in 2014 using data from the “IDA Study” (Dementia Care Initiative in Primary Practice). On average, the 351 informal caregivers (CGs) were 59.2 years old (SD = 13.4), 73% were women, 31% were spouses, 60% were children (in-law), and 9% were other CGs. The average age of those suffering from dementia was 80.3 years (SD = 6.7), and 68% of them were women. Sixty four percent suffered from a mild form of dementia (Mini Mental State Examination (MMSE): 18-24 points; Folstein et al., 1975) and 36% from a moderate form (MMSE: 10-17 points). Cronbach’s alpha was calculated to determine the internal consistency of the items. An exploratory factor analysis was used to determine the correlation structure of the BSFC-s. In addition, the discriminatory power, item difficulty, and construct validity were examined by testing five hypotheses.
In order to assess the validity of the scale, we analyzed additional information about the severity of dementia (MMSE), demanding behaviors of dementia patients (Nurses’ Observation Scale for Geriatric Patients (NOSGER); Spiegel et al, 1991), the depression diagnosis of caregiving relatives (ICD-10 diagnosis, taken from health insurance data), the care level, the degree of care-recipient’s functional independence (Barthel Index; Mahoney, 1965), the care activities at night, the time required for informal care in hours per day (Resource Utilization in Dementia – Lite Version (RUD Lite); Wimo & Winblad, 2003), and sociodemographic and general characteristics.
Construct validity was tested and confirmed on the basis of five hypotheses (H1-H5). The results are presented in Table 2 in Grau and Graessel (2015).
- H1: The burden on CGs is positively correlated with the severity of cognitive impairment, which was measured with the MMSE.
- H2: Demanding behaviors (operationalized with the NOSGER “disruptive behavior” subscale) are among the most distressing symptoms associated with dementia. The burden on CGs is positively correlated with the severity of the challenging behaviors.
- H3: The burden on CGs is related to their mental health, that is, CGs with a diagnosis of a depressive episode have higher subjective burden scores than CGs without this diagnosis.
- H4: CGs who have only limited opportunities for retreat report a higher burden of care, that is, CGs who share an apartment/house with the person in need of care have a higher burden of care than those who live separately.
- H5: The more demanding the care requirement, the greater the burden on the CG.
- H5a: The higher the care level, the greater the burden on the CG.
- H5b: The lower the degree of independence of the care-recipient (measured with the Barthel Index), the greater the burden on the CG.
- H5c: The more care tasks are carried out at night, the greater the burden on the CG.
- H5d: The higher the average daily care effort in hours, the higher the CG´s workload.
Predictive validity was confirmed on the basis of H6: The higher the burden on the CG(s), the more likely it was that the care-recipient would be institutionalized in the future (transferred to a nursing home). All predictors are presented in Table 3 in Graessel et al. (2014).
Internal consistency: Cronbach’s alpha was .915.
The item difficulty of the items of the BSFC-s ranged from .16 to .40. All 10 items showed a high discriminatory power between .55 and .75. For all 10 items, the Cronbach’s alpha value “when the item was removed” was below the Cronbach’s alpha for the complete scale of .915. The results are presented in Table 1 in Graessel et al. (2014).
The exploratory factor analysis revealed a one-factor structure of the BSFC-s: Only one factor had an eigenvalue greater than 1.0 (eigenvalue = 5.69). This factor explained 57% of the total variance of the BSFC-s sum score. Each of the 10 items loaded on this factor with factor loadings greater than .60.
The scree plot shows the distribution of the eigenvalues of the calculated factors and confirmed the one-factor structure of the BSFC-s:

Folstein, M.F., Folstein, S.E. & McHugh, P.R. (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189-198.
Graessel, E., Berth, H., Lichte, T. & Grau, H. (2014). Subjective caregiver burden: validity of the 10-item short version of the Burden Scale for Family Caregivers BSFC-s. BMC Geriatrics, 14, 1-9.
Mahoney, F.I. & Barthel, D.W. (1965). Functional evaluation: the Barthel Index. Maryland State Medical Journal, 14, 61-65.
Spiegel, R., Brunner, C., Ermini-Fünfschilling, D., Monsch, A., Notter, M., Puxty, J. & Tremmel, L. (1991). A new behavioral assessment scale for geriatric out-and-in-patients: the NOSGER (Nurses´Observation Scale for Geriatric Patients). Journal of the American Geriatrics Society, 39(4), 339-347.
Wimo, A. & Winblad, B. (2003). Resource utilization in dementia: RUD Lite. Brain Aging, 3(1), 48-59.
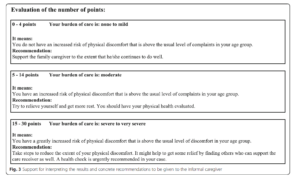
An extended validation study was carried out in 2018 using data from 386 CGs for various causes of care dependency. On average, the CGs were 61.3 years old (SD = 12.2), 76% were women, 35% were spouses or partners, 60% were children (in-law), and 3% were other CGs. Only 1% had no family connection. Cronbach’s alpha was calculated to examine the internal consistency of the items. Convergent validity was also determined. A valid classification system was developed on the basis of the Giessen Complaints Questionnaire (GBB-24; Brähler et al., 2008), which facilitated the interpretation of the BSFC-s sum value.
The following instruments were used to test convergent validity: GBB-24 (Brähler et al., 2008), Caregiver Strain Index (CSI) (Robinson, 1983), Berlin Inventory of Caregivers’ Burden with Dementia Patients (BIZA-D) (Zank et al., 2006), Care-related Quality of Life Instrument (CarerQoL) (Brouwer et al., 2006), Patient Health Questionnaire (PHQ-9) (Gräfe et al., 2004).
Internal consistency: Cronbach’s alpha was .92.
The correlations between the BSFC-s and the other measurement instruments confirmed the convergent validity:
| HPS-k | |
| Caregiver Strain Index (CSI) | r = .70, p < .001 |
| Care related Quality of Life Instrument (CarerQoL) | r = − .72, p < .001 |
| Giessen Subjective Complaints List (GBB-24) | r = .68, p < .001 |
| Patient Health Questionnaire (PHQ-9) | r =.68, p < .001 |
| Berlin Inventory of Caregivers´ Burden With Dementia Patients (BIZA-D) | r = .16, p = .002 |
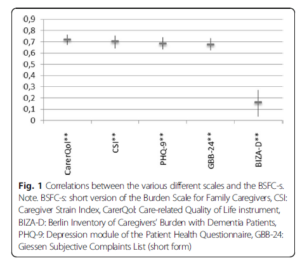
Based on the risk of psychosomatic physical complaints, the severity of which (not increased, increased, greatly increased) was directly related to the extent of subjective care-related stress, the BSFC-s sum value can be interpreted with valid content.
Brähler, E., Hinz, A. & Scheer, J.W. (2008). GBB-24. Der Gießener Beschwerdebogen: Manual. Hans Huber.
Brouwer, W.B.F., Van Exel, N.J.A., Van Gorp, B. & Redekop, W.K. (2006). The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Quality of Life Research, 15, 1005-1021.
Gräfe, K., Zipfel, S., Herzog, W. & Löwe, B. (2004). Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)”. Diagnostica, 50(4), 171-181.
Gräßel, E., Berth, H., Lichte, T. & Grau, H. (2014). Subjective caregiver burden: validity of the 10-item short version of the Burden Scale for Family Caregivers BSFC-s. BMC Geriatrics, 14, 1-9.
Pendergrass, A., Malnis, C., Graf, U., Engel, S. & Graessel, E. (2018). Screening for caregivers at risk: Extended validation of the short version of the Burden Scale for Family Caregivers (BSFC-s) with a valid classification system for caregivers caring for an older person at home. BMC Health Services Research, 18, 1-9.
Robinson, B.C. (1983). Validation of a caregiver strain index. Journal of Gerontology, 38(3), 344-348.
Zank, S., Schacke, C. & Leipold, B. (2006). Berliner Inventar zur Angehörigenbelastung-Demenz (BIZA-D). Zeitschrift für klinische Psychologie und Psychotherapie, 35(4), 296-305.
The BSFC-s has been validated in the following languages: Arabic, Japanese, Malay, Urdu.
You can find the corresponding validation studies here.
Burden Scale for Family Caregivers (BSFC); Burden Scale for Family Caregivers – short form (BSFC-s); Informal Caregiver (CG); Arithmetic mean (M); Standard deviation (SD)
